Originally Published in 2016
Consciousness and Concussion
by Ralph B. Lilly, M.D. | Contributor
Of all the organs in the body, the brain is, to me, the most fascinating. It is so complex in some respects but in others so simple. Nestled within our skull, the brain is composed of billions of cells called neurons. Each one is organically wired through a complex array of thousands of connections to transmit electromagnetic impulses to other neurons. Together with the supporting cells and blood vessels, the brain contains all the electrolytes and chemicals necessary for survival of the entire nervous system. Those signals affect how we think, move and interact in our environment every day.
What is Consciousness?
Those electromagnetic wave forms in our brain produce the complex functions that we describe as “consciousness.” We learned as children about the five senses (smell, taste, vision, hearing and touch), which are components of the brain’s many responsibilities. In reality, there are other sensations, such as our ability to orient ourselves in space and three-dimensional perception. Our senses generate our emotions like fear, joy and sadness. Our responses are based on all the information we are continually taking in, and our brains have to make judgments and decide on actions to take 24 HOURS A DAY.
So…the brain is the essential organ of consciousness. And, because we are all unique individuals, our behaviors are equally unique. The memories contained in our neural network are constantly in a state of change. It’s like electronic storage of all of our prior conscious experiences, our learning, and our sensory and motor experiences. All of these are transformed to become our individual responses to external stimuli. The way your brain takes in all that information and how it chooses to respond is individual to YOU.
What is Concussion?
Concussion is considered a transient alteration in these brain functions. Many in the medical community have chosen to use the term concussion as a replacement for the term “mild traumatic brain injury” because there is NO brain injury that should be considered “mild,” especially for the victim, family, friends, employers, and the community.
The brain can suffer trauma in many ways, but the dynamics of the impact to the skull or of the brain slamming against the inside wall of the skull as it accelerates and decelerates cause the physical symptoms patients experience. The damage caused to the brain impacts the way the nervous system is able to function.
Whenever a patient has had a period of time in which the level of arousal has been affected, it is termed “unconscious.” The injured person may not have even been aware of it, or it may even be so brief that others don’t witness it. So, a loss of consciousness is not required to make the diagnosis of concussion. There is, however, often a “confusional state” when the patient demonstrates impairments in memory, attention, concentration, perception, judgment, personality, emotion and decision-making.
The patient may also experience dizziness, headache, ringing in the ears, imbalance, fatigue, difficulty initiating activity, persistent headache and feelings of “fogginess.” If a combination of these symptoms exists for more than 24 hours, the patient is considered to have “post-concussive syndrome.” The cognitive and behavioral changes may persist for variable amounts of time depending on the nature of the trauma and on the individual’s own brain.
How Do We Manage Concussions?
Because the brain consists of so many microscopic neuronal connections, damage to the brain’s tiniest components may be difficult or impossible to see on traditional MRI and CT scans. Diagnostic imaging may show negative findings, but that should NOT always be interpreted to mean that there has been no injury. The patient and his or her caregivers have to carefully consider the symptoms as well.
Medical management of concussion requires early evaluation by (pediatric) neurologists, pediatricians, physiatrists and neuropsychologists. The diagnostic studies should include imaging as well as neuropsychiatric assessment. It’s important to inform and work with the patient’s school system or employer, family members and caregivers.
Some patients require accommodations to their school or work schedules. Speech, occupational, cognitive, vocational and avocational therapies can help to address individual needs. Those therapists and physicians should provide guidance regarding sleep, diet, exercise and especially—how to avoid further cranial trauma.
Concussion should be considered a serious brain injury. While it is not necessarily associated with a direct threat to someone’s life, it is commonly associated with significant alterations to the injured person’s daily life. With the proper attention and intervention, the outlook is invariably improved.
The Centers for Disease Control and Prevention estimated that 1.7 million traumatic brain injuries occurred on average each year in the U.S. during 2002 to 2006. Of these brain injuries, 45,000 to 50,000 people do not survive. Roughly 50% of the survivors may return to baseline functioning in 6 months. After the first year post-trauma, approximately 85% return to pre-traumatic function. After one year, however, there will remain 10%-15% of the brain injured, who will have residual problems of varying degrees. These problems can range widely and include memory problems, anger outbursts, alteration of personality and negative impact upon day-to-day functioning. These problems could last a lifetime, with variable persistent impairments and handicap. If these symptoms persist, Post Traumatic Encephalopathy then becomes the diagnostic term, implying persistent pathological changes to the brain
Roughly 200,000 patients with concussion with varying persistent impairments of brain function enter the health care population each year. Even those who recover within one year have required months of extensive therapy following the trauma. Patients with the poorer outcome include patients with a history of prior brain injury, those who had sustained other injuries such as to the face, jaw, eye, ear, neck, skull and other organ systems.
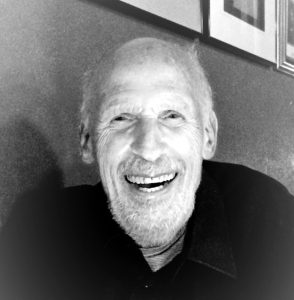
Editor’s Note: In addition to being a renowned physician and acclaimed brain specialist, Dr. Ralph Lilly was also my Uncle Ralph, the big brother to my Dad, Earle Lilly.
Dr. Lilly passed away in 2021 before he could finish his book about the Healers — the family, friends, and companions who stand beside brain injured people and help usher them to new, often different, often better, lives. But, his co-author, Diane F. Kramer, carried the torch, and recently announced that their book, “Second Lives: The Journey of Brain-Injury Survivors and their Healers,” has just been published.
Additional articles you might find interesting:
High School Trainers Use Know How and Imaging to Keep Players in the Game
Doctors’ Tips for a Healthier Life
Ralph B. Lilly, M.D.
October 28, 1935-October 10, 2021
About Ralph Lilly, M.D.
Dr. Lilly grew up in Revere and Chelsea, Massachusetts and graduated from Revere High School in 1952. He was 6’4” so when he attended undergraduate studies at Brandeis University, he was recruited for football, but never liking violence or physical confrontation, he quit the team, but stayed active in an administrative capacity.
Graduating from Brandeis, he took a job as a Chemistry teacher and basketball coach in St. John, New Brunswick. After a year, he entered Dalhousie Medical School in Halifax, Nova Scotia and from there to Phoenix, AZ for a residency at The Barrow Neurologic Institute, then into private practice.
His life changed in 1980, when, on his motorcycle and stopped at a red light, he was run down by a drunk driver. Both he and the person on the bike were severely injured and that traumatic brain injury brought Ralph to a new life and career.
After not working for two years, he entered a Fellowship at UCLA tailored for him by the Chair of Neurology, Dr. Frank Benson, a pioneer in Neurobehavior. Working with Dr. Benson and with Dr. Jeff Cummings at UCLA for a year he learned about the brain and what can happen to it and to behavior when it is damaged. This experience brought Ralph to the grand road of Neurobehavior.
From LA he journeyed to Providence, Rhode Island where he took a position as the Director of Neurological Services at Butler Psychiatric Hospital, associated with Brown University Program in Medicine.
Dr. Lilly was instrumental in teaching the medical and nursing staff at Butler and other facilities in Rhode Island and Massachusetts about Neurobehavior and the consequences of Acquired Brain Injury.
After 9 years at Butler, Dr. Lilly Ralph headed to Houston, TX, treating more acutely injured patients with Dr. John Cassidy at the Neurobehavioral Institute of Houston. Gaining incredible experience with Dr. Cassidy, Ralph interacted with hundreds of patients and families, being there not only for medical treatment, but offering psychological support.
Ralph was the first Medical Director of the Houston Polo Club, and set up a system to quickly intervene with any injuries on the field, and transport to emergent care, if needed.
Eventually Dr. Lilly found the door to the University of Texas at the Houston Medical Center, Department of Neurosurgery opened to him by the Chief of Neurosurgery, Dr. Guy Clifton. Working first with Dr. Clifton and his Neurosurgeons, Ralph eventually saw patients on all of the ICUs at Memorial Hermann Hospital in Houston.
Dr. Lilly’s focus in the last decade came to be on his outpatient clinic in Houston. He saw patients and families whether they could pay or not. He had knowledge, empathy and love to share and that is what he did.
Throughout his many years of practice, Dr. Lilly was instrumental in saving so many lives, with his skill, his patience, his perseverance in the face of seemingly unsurmountable problems.
Dr. Lilly strived to finish his book about the Healers — the family, friends, and companions who stand beside brain injured people and help usher them to new, often different, often better, lives. He died before he could see the book to fruition, but his co-author, Diane F. Kramer, carried the torch. The book, Second Lives: The Journey of Brain-Injury Survivors and their Healers, has just been published.